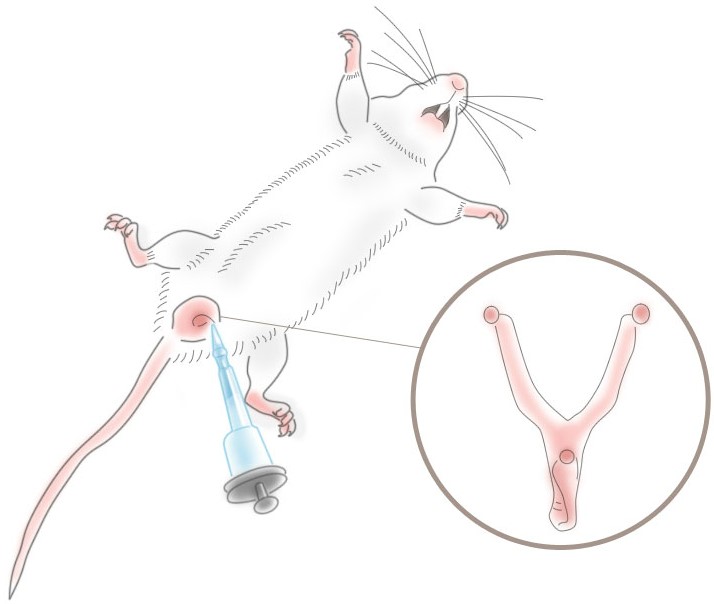
Instilling Clodronate Liposomes into the Vagina
As with the nasal, pulmonary and other mucosal surfaces, the vaginal mucosum must defend the animal from invasion by external pathogens and other foreign particles. Therefore various immune-responsive phagocytic cells are present in order to remove and kill invading pathogens as well as to initiate antibody production to further protect the animal from future attacks whenever possible. Like all other phagocytic cells, vaginal phagocytes identify liposomes as foreign particles and remove them via phagocytosis. Internalized clodronate liposomes kill the phagocytes which will, in turn, release cytokines into the bloodstream thus recruiting new phagocytes to the site of the invasion. This means that the experimental protocol must take into account the fact that the depletion of the local phagocytes is temporary and additional systemic (i.p. or i.v.) clodronate liposome dosing will be necessary if prolonged vaginal phagocyte depletion is the goal.
Direct instillation of clodronate liposomes into the vagina has been reported in only 1 paper, and until these results were published, it was only an assumption that local vaginal phagocytes (macrophages and dendritic cells) could be depleted by direct intravaginal instillation of clodronate liposomes. Although not addressed specifically in this paper, it is a further assumption that the phagocyte depletion after intravaginal instillation is limited to the vaginal tissue, although transport to local lymph nodes should be investigated.
Although the importance of cytotoxic T lymphocytes and neutralizing antibodies for antiviral defense is well known, the antiviral mechanism of Th1 remains unclear. We show that Th1 cells mediate noncytolytic antiviral protection independent of direct lysis through local secretion of IFN-γ after herpes simplex virus-(HSV) 2 infection. IFN-γ acted on stromal cells, but not on hematopoietic cells, to prevent further viral replication and spread throughout the vaginal mucosa. Importantly, unlike other known Th1 defense mechanisms, this effector function did not require recognition of virally infected cells via MHC class II. Instead, recall Th1 response was elicited by MHC class II + antigen-presenting cells at the site of infection. Dendritic cells (DCs) were not required and only partially sufficient to induce a recall response from memory Th1 cells. Importantly, DCs and B cells together contributed to re-stimulating memory CD4 T cells to secrete IFN- γ . In the absence of both DCs and B cells, immunized mice rapidly succumbed to HSV-2 infection and death. Thus, these results revealed a distinct mechanism by which memory Th1 cells mediate noncytolytic IFN-γ–dependent antiviral protection after recognition of processed viral antigens by local DCs and B cells.
Technical Notes
- HSV-2 immune mice were dosed with clodronate and control liposomes intravaginally (10 µl) and i.p. (250 µl) on days -4 and -2 prior to HSV-2 re-challenge on day 0.
- No details of intravaginal instillation method published.