Direct Administration of Clodronate Liposomes into the Cerebrospinal Fluid (CSF) and other Brain Tissue
The brain protects itself from blood-borne pathogens and toxins by severely restricting the transport of cells, particles and most hydrophilic molecules across the vascular endothelium of blood vessels in the brain. This protective mechanism is known as the blood-brain barrier, or BBB. Even hydrophobic molecules which can cross the endothelial cell membranes are frequently pumped back into the bloodstream by astrocytes closely associated with the endothelium. Blood-borne molecules which the brain requires for metabolic functions (glucose, amino acids) or systemic signal/response mechanisms (insulin, neurotransmitters) each have specific transporters for brain uptake. These transport mechanisms are often utilized for pharmacological intervention by identifying active analogs (L-DOPA) of the naturally transported molecules that can take advantage of the transporters. Some systemic vasodilators (bradykinin) or administering i.v. mannitol to increase the osmotic strength of the blood can briefly increase the BBB permeability.
Unlike other vascular endothelia, the BBB does not respond significantly to low-level systemic inflammatory signals but certain infectious diseases (bacterial/viral meningitis) and neurological diseases (multiple sclerosis) that affect the brain itself, or intracrainial hemorrhage (from physical injury or stroke), can result in local breaches in the BBB due to the inflammatory response within the brain. These pathological states can result in increased access by antibiotics and other drugs which may assist in restoring brain health, however the infiltration of monocytes and other blood components have also been associated with increased damage to the brain [1, 2]. Conversely, some scientists have postulated and demonstrated that infiltrating monocytes can be loaded with drugs (i.e. via liposomes) for beneficial delivery to the brain and others have designed liposomes to directly cross the BBB [3].
Microglia are the resident inflammatory cells within the brain. Like macrophages and monocytes, they are of myeloid origin (entering the brain tissue during fetal and post-natal development) where much of their protective function is effected by phagocytosis [4]. Moreover, microglia are also implicated in many CNS disease states [5]. Several groups have demonstrated microglial depletion using clodronate liposomes, thus they can play a major role in elucidating the functions and effects of these phagocytes just as they have in thousands of studies involving systemic phagocytes. Analogous to the systemic cast of immune cell types (macrophages, dendritic cells, etc. and their sub-classes), the CNS includes a variety of immune cells (perivascular macrophages, meningeal macrophages, choroid plexus macrophages, dendritic cells, etc.) many of which may also be depleted by clodronate liposomes.
Although several studies on CNS inflammatory mechanisms and pathologies have utilized intravenously dosed clodronate liposomes, effective depletion of the microglia and other CNS phagocytes requires the liposomes to be administered directly into the cerebrospinal fluid. Unlike the systemic circulation in which liposomes have multiple opportunities to be either phagocytosed or extravasate through fenestrated epithelia, the CSF flow is unidirectional from the lateral ventricles through 0ther 3rd ventricle into the 4th ventricle which empties into the cisterna magna where it is distributed over the outer surface (subarachnoid space) of the brain. CSF is initially derived from the blood through the specialized structure of the choroid plexus. This means that CSF is blood serum that has been filtered across the BBB which excludes all cells, particles and molecules except those which have specific transport systems as discussed above. Choroid plexus formations are found in each of the ventricles, therefore CSF is generated in the ventricles from where it flows unidirectionally into the subarachnoid space. From here the CSF is reintegrated into venous blood through the arachnoid villi or arachnoid granulations (click here to view video describing the generation and flow of CSF through the human brain from the McGraw-Hill teaching website). Therefore, liposomes which are not phagocytosed in their maiden journey through the ventricular and cisternal spaces of the brain will be delivered into the venous blood. This explains why some scientists report systemic phagocyte depletion post-injection of clodronate liposomes into the CSF as well as why the selection of the injection site in the brain is extremely important. In fact, Pardridge likens injection into the CSF to a slow i.v. infusion which is supported by several studies [6]. He further cites studies which show that labelled growth factors and other molecules do not penertrate the brain parenchyma even when administered directly into the CSF. Therefore, the barrier between the CSF and the brain tissue is just as occlusive as that between the blood vessels and brain parenchyma meaning that local phagocytes or other methods for cell penetration must also be utilized to access brain tissue even from the CSF.
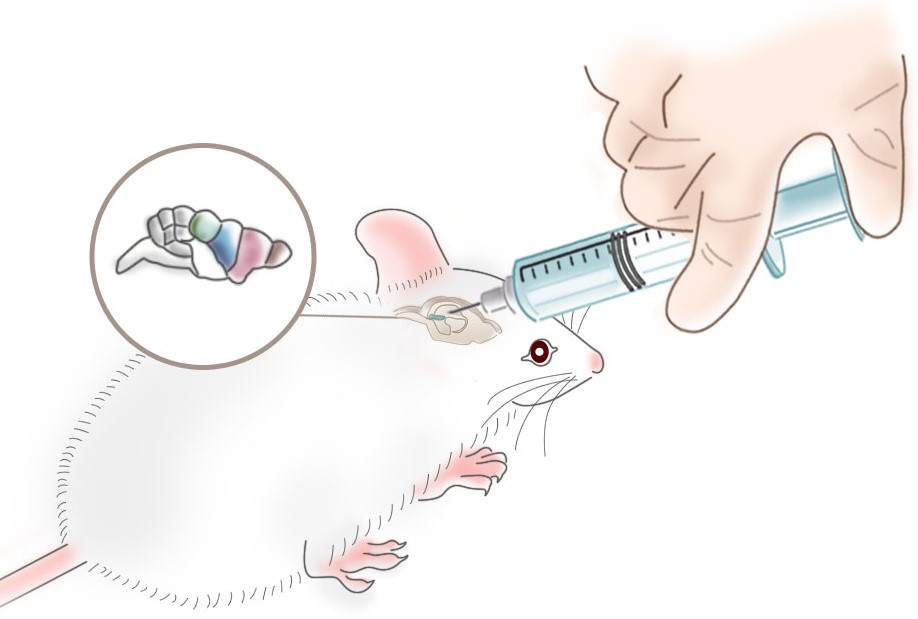
The two most cited routes for injecting clodronate liposomes into the CSF is intracisternal (i.c., i.cist, i.cis) and intracerebroventricular (also referred to as intraventricular or ICV), although one study describes direct injection of clodronate liposomes into the tissue of the hippocampus [7]. Whichever route is chosen, the injection rate should be very slow so as not to induce a sudden increase in the intracranial pressure due to the increase in CSF volume. The projectile used for the injection should also be left in place for a few minutes post-delivery then retracted very slowly in order to prevent the CSF backflow through the injection canal. Control animals injected with saline should be closely observed after the injection in order to identify and/or differentiate any reactions due to possible brain disruption or damage from the injection itself.
The intracisternal route most commonly indicates that the injection is into the cisterna magna at the base of the skull, although Chiavolini, et al. developed a technique for establishing a meningitis model in which the injections access the cisterns in the subaracnoid space which they refer to as i.c. subarachnoidal [8]. Surprisingly, their histological data indicates that this injection route also allowed dye to penetrate the lateral ventricles which would be contraindicated if the dye was indeed delivered into a subarachnoid cistern assuming that the flow of the CSF proceeds unidirectionally from the ventricles into the cisterna. This is possibly due to differences between human and mouse brain structure. This injection route was established stereotaxically [9, 10] which means that the needle is inserted at a specific location to a specific depth (using x,y,z coordinates) where the target site is located based on a 3-dimensional model of the brain. The accuracy of the injection is then verified histologically sometimes with the aid of dye. A video of this technique is included in the Geiger, et al., paper [11]. The intrahippocampal injection was also accomplished using stereotaxic vectors for locating the hippocampus within the rodent brain.
Likewise, intracerebroventricular injection methods are often described steriotaxically and histological verification of the accuracy of the injection is also required to generate reliable data. Given the unidirectional CSF flow, the maximal exposure of brain surface to liposomes in the CSF is accomplished by liposome injection into both lateral ventricles as described in Galea, et al . [12]. After failing to deplete perivascular macrophages (PVM) in the brain by adapting the published method for rat PVM depletion (injection into the 4th ventricle), the authors injected the liposomes into both lateral ventricles resulting in complete depletion of mannose-receptor positive (MR) cells. Assuming that injection into the 4th ventricle precludes liposome access to the lateral and 3rd ventricles, this result is not surprising. Again, however, there may be interspecies variations in brain structure and CSF flow which may require injection site adjustments to accomplish the desired results. This further emphasizes the need to verify the success of the injection to the intended site as well as establishing the optimal dose, dosing schedule and time post-injection required for maximal macrophage depletion.
Along with validating the method used for phagocyte depletion, it is extremely important that control liposomes (without encapsulated clodronate) be dosed to a group of animals especially when cytokine measurements and evaluation of the activation state of the macrophages are included in the protocol. As discussed for one of the papers below, a free clodronate control is also an important group to include since it is likely that some clodronate is released from the liposomes when they are introduced into the CSF. It is also advisable to assess the effect of free clodronate added to empty liposomes at least in a few animals especially when confounding data has arisen from initial experiments.
Given that less than 15 papers have been published on the application of clodronate liposomes in the depletion of phagocytes in the brain in three different species, optimization and validation of the clodronate liposome phagocyte depletion model along with careful attention to the control groups incorporated into the studies will, no doubt, prove to be a most productive and scientifically unique arena for studying the immunological behaviors and mechanisms in the CNS. Perhaps even more importantly, most CNS diseases are linked to immunological and inflammatory reactions, therefore many therapeutic modalities will result from these efforts as well.